This article is written by Dr. Bilal Raees Qureshi, a practicing dentist with 8+ years of experience at Z Care Dental Experts.
Toothaches are often brushed off as minor nuisances. Maybe you take a painkiller, swish with some warm saltwater, and hope it passes. But here’s the alarming truth: A tooth infection left untreated can escalate into a medical emergency. Some infections can spiral out of control in just a few days, causing life-threatening complications.
When people ask, How long until a tooth infection kills you?, they’re not exaggerating. While not every abscess leads to tragedy, there have been real cases where healthy young people lost their lives. What started as nothing more than a toothache quickly became an infection that spread out of control.
I still remember reading about a 26-year-old truck driver from Sacramento who lost his life because of a tooth infection. At first, it was just a bad toothache that he tried to ignore while working long hours on the road. He didn’t go to the dentist because of the cost and thought painkillers would be enough. But within days, the infection spread to his jaw and bloodstream, making it impossible to control. By the time he finally reached the hospital, doctors couldn’t save him, and something so small ended his life far too soon. Such cases underscore why understanding the risks and acting quickly is so important.
This article will explore how tooth infections form, how fast they spread, and the warning signs you should never ignore. You’ll also learn about treatments, prevention, and lifestyle choices that protect your teeth and overall health.
What Is a Tooth Infection?

Definition and Causes
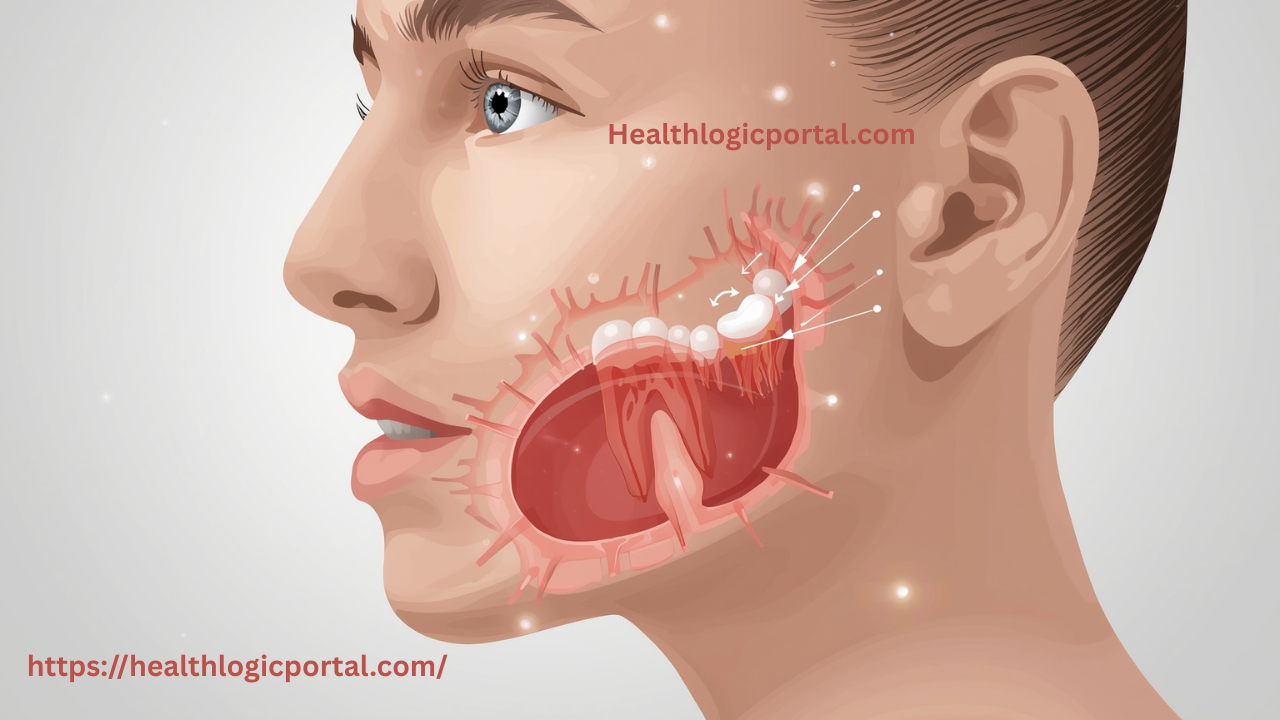
A tooth infection, also called a dental abscess, occurs when bacteria invade the innermost part of the tooth. Normally, enamel and dentin shield the pulp (which houses nerves and blood vessels) from bacterial attack. But bacteria move in when tooth decay, trauma, or gum disease compromises these protective layers.
Common causes include:
- Untreated cavities: The number one trigger for infections.
- Cracked or chipped teeth: Open pathways for bacteria.
- Advanced gum disease (periodontitis): Weakens the surrounding tissues.
- Poor dental hygiene: Skipping brushing and flossing allows plaque buildup.
Left unchecked, bacteria thrive in the pulp chamber, forming pus and painful swelling.
Types of Dental Abscesses
Not all tooth infections are the same. Dentists usually categorized them into three types:
- Periapical Abscess: Forms at the root tip due to deep cavities or trauma.
- Periodontal Abscess: Originates in the gums, often from untreated gum disease.
- Gingival Abscess: Limited to the gum tissue, typically less severe but still painful.
Each of these can spread if untreated. What begins as localized discomfort may evolve into facial swelling, difficulty swallowing, and, in extreme cases, systemic infection.
How Fast Can a Tooth Infection Spread?
A big part of the danger lies in how unpredictable infections can be. Some smoulder for weeks, while others become dangerous overnight.
Early Stage (First 24–72 Hours)
During the initial days, you’ll likely experience throbbing tooth pain, sensitivity to hot and cold, and tenderness around the gums. Swelling may begin, but usually, the infection hasn’t spread beyond the tooth yet.
When It Moves Beyond the Tooth
If ignored, bacteria infiltrate nearby structures gums, jawbone, and facial tissues. This is when swelling intensifies, and you may see puffiness around the jaw or under the eyes. Pain often radiates, making it feel like your entire face is throbbing.
The Role of the Immune System
How quickly this process unfolds depends heavily on your body’s defences. A strong immune system may slow bacterial progression, but if your immunity is compromised, whether from diabetes, smoking, or stress the, infection can spread rapidly.
This is why two people with the same type of abscess can have completely different outcomes: one may deal with localized pain for weeks, while another ends up hospitalized within days.
Can a Tooth Infection Kill You?
It’s a chilling thought, but yes, a tooth infection can be fatal if left untreated. Modern dentistry and antibiotics make deaths rare today, but the possibility still exists.
How Infections Reach Vital Organs
Dental infections spread through two main routes:
- Bloodstream (sepsis): Bacteria enter circulation, potentially reaching the heart, kidneys, or other organs.
- Soft tissue spread: Abscesses extend to the neck or jaw, sometimes compromising the airway.
Real Dangers: Sepsis, Ludwig’s Angina, Brain Abscess
- Sepsis: A body-wide inflammatory response that can cause organ failure.
- Ludwig’s Angina: Severe neck swelling that may block breathing.
- Brain Abscess: Rare but deadly when infection spreads upward from upper teeth.
Historical vs. Modern Outcomes
Before antibiotics were widely available, dental infections were among the top causes of death. Today, while fatalities are uncommon in developed countries, people without access to prompt care due to cost, location, or neglect remain at risk.
Symptoms That Signal Danger
How do you know when a tooth infection crosses the danger zone? Pay close attention to these symptoms:
Common Signs of a Simple Abscess
- Persistent toothache (sharp or throbbing)
- Swelling of the gums
- Sensitivity to hot and cold
- Bad taste in the mouth due to pus leakage
Red Flags That Indicate Spreading Infection
- Rapidly increasing facial or neck swelling
- Fever, chills, or body aches
- Difficulty swallowing or breathing
- Swollen lymph nodes
- Extreme fatigue or dizziness
When to Go to the ER vs. the Dentist
- Dentist appointment: For localized swelling and pain without fever or difficulty swallowing.
- Emergency room: If you have a fever, trouble breathing, or rapidly spreading swelling, these are signs that the infection is beyond dental management alone.
How Long Until a Tooth Infection Becomes Fatal?

When people ask, How long until a tooth infection kills you? The honest answer is—it depends. There isn’t a universal timeline because infections behave differently in each person. However, understanding the possible progression gives a clearer picture.
Why Timelines Vary by Patient
Several factors influence how fast an infection can spiral:
- Overall health: A strong immune system can hold off bacteria longer, while those with weakened immunity may deteriorate faster.
- Location of infection: Upper jaw infections spread more easily to the brain, while lower jaw infections may spread to the neck and airway.
- Access to care: Someone who can see a dentist quickly will avoid dangerous complications.
Typical Progression From Infection to Complication
- First 1–3 days: Localized tooth pain, swelling around the gums, and tenderness when chewing.
- Day 3–7: Swelling may spread to the cheek or jaw, pus drain, and fever appear.
- 1–2 weeks untreated: Bacteria can spread to facial spaces, airway, or bloodstream. Symptoms escalate—difficulty breathing, swallowing, or speaking clearly.
- Beyond 2 weeks: Life-threatening complications like sepsis, Ludwig’s angina, or brain abscess may develop.
Treatment Options for a Tooth Infection
The good news is that tooth infections are highly treatable if addressed early. Modern dentistry provides several solutions depending on the severity.
Antibiotics and Why They’re Not Enough
Antibiotics are often the first step in controlling bacterial spread. They help reduce swelling and fever, but can’t remove the source of infection. The bacteria may resurface once the antibiotic course ends unless the tooth is treated.
Drainage and Root Canal Therapy
- Drainage: Dentists may make a small incision in the gum or tooth to release pus, relieving pressure and pain.
- Root canal therapy is the gold-standard treatment for saving an infected tooth. The dentist cleans the infected pulp, disinfects the canals, and seals the tooth to prevent reinfection.
Extraction as a Last Resort
If the tooth is too damaged, extraction may be the safest option. While losing a tooth isn’t ideal, it prevents the infection from spreading further.
Emergency Interventions
In extreme cases where the infection has spread to the neck or airway patients may require hospitalization, IV antibiotics, or surgical procedures to clear infected tissue.
Can Home Remedies Help?
When faced with tooth pain, people often turn to home remedies, hoping to avoid a dental visit. While some remedies can provide temporary relief, they cannot cure an infection.
Temporary Relief Options
- Warm saltwater rinses: Reduce swelling and flush bacteria from the gum area.
- Cold compresses: Help with pain and facial swelling.
- Over-the-counter pain relievers: Ibuprofen and acetaminophen can ease discomfort until treatment.
Myths and Dangerous Remedies to Avoid
- Applying alcohol directly to the tooth can burn the gums without treating the infection.
- Puncturing the abscess at home: Risk of spreading bacteria further into the tissues.
- Relying solely on herbal remedies: Herbs may soothe pain but don’t eliminate bacteria.
Role of Diet and Natural Healing
While no food can “cure” an abscess, a nutrient-rich diet supports immune function and healing. Just as certain natural foods like honeycomb or water apple provide antioxidants and antimicrobial compounds that benefit overall wellness, maintaining balanced nutrition can make your body more resilient against infections.
Preventing Tooth Infections Before They Start
Prevention is far easier and cheaper than dealing with a severe infection. Consistent oral hygiene and smart lifestyle choices make a huge difference.
Daily Oral Hygiene Practices
- Brush at least twice a day using fluoride toothpaste.
- Floss daily to remove plaque between teeth.
- Use an antimicrobial mouthwash to kill lingering bacteria.
Diet and Nutrition for Dental Health
- Best foods: Dairy for calcium, leafy greens for vitamins, and crunchy fruits/veggies that stimulate saliva.
- Worst foods: Sugary snacks, sodas, and sticky candies that cling to enamel.
Eating whole, fresh foods benefits your teeth and supports gut and systemic health. In fact, many experts recommend natural juices for digestive balance—like those discussed in the best juice for gut health to keep your body stronger overall.
Importance of Regular Dental Check-ups
Visiting your dentist every 6 months ensures early detection of cavities, gum disease, or cracks before they become infections. Your dentist may recommend more frequent monitoring if you’ve had recurrent abscesses.
How Diet Affects Oral and General Health

It directly impacts your teeth, gums, and risk of infections.
Foods That Support Healthy Teeth
- Calcium-rich foods: Milk, cheese, yoghurt strengthen enamel.
- Vitamin C sources: Oranges, kiwis, peppers promote gum health.
- Water-rich fruits: Apples, cucumbers, and melons wash away food particles.
Harmful Foods That Increase Infection Risk
- Sugary sodas and energy drinks erode enamel.
- Processed carbs break down into sugars, feeding bacteria.
- Alcohol and smoking dry out the mouth, reducing saliva’s protective effect.
Links to Systemic Health
A poor diet affects more than just your smile—it impacts your whole body. Scientists have linked gum disease to systemic conditions like heart disease and diabetes [source]. Supporting oral health with nutritious foods can lower the risk of infections spreading beyond the mouth.
For example, omega-3-rich fish like red snapper reduce inflammation in both gums and the cardiovascular system, showing how interconnected dental and general health are.
Risk Factors That Make Infections More Dangerous
Not everyone faces the same level of risk regarding dental infections. For some people, what starts as a minor abscess can quickly become life-threatening due to underlying health or lifestyle factors.
Diabetes and Immune Disorders
People with diabetes, HIV, or other immune-compromising conditions are at higher risk. Their bodies struggle to fight off infections, giving bacteria more time to spread. Even a small abscess can escalate rapidly in these individuals. For diabetics, high blood sugar also fuels bacterial growth and slows healing.
Smoking and Alcohol Use
Tobacco and alcohol both weaken oral tissues and reduce the body’s immune response. Smokers are twice as likely to develop gum disease, which makes abscesses more common. Alcohol, meanwhile, can cause dehydration, lowering saliva production—the mouth’s natural defence mechanism against bacteria.
Age and Access to Care
- Older adults: More prone to chronic illnesses and may have difficulty accessing dental care.
- Children: Their infections can progress quickly, particularly if cavities are untreated.
- Underserved populations: People without dental insurance or living in rural areas often delay treatment, putting them at greater risk of complications.
In short, while anyone can die from a tooth infection, certain groups need to be especially vigilant.
Living With Chronic Dental Issues
Some people experience repeated dental infections, which may signal deeper oral health concerns.
Recurrent Abscesses and What They Mean
If abscesses pop up every few months, it’s a red flag. It may indicate:
- Unfinished root canal therapy
- Advanced gum disease
- Poor oral hygiene habits
- Underlying systemic health issues (like diabetes)
Long-Term Management Strategies
- Comprehensive dental evaluation: To uncover the root cause of recurrent infections.
- Regular cleanings: Professional cleanings every 3–4 months if you’re prone to gum disease.
- Lifestyle adjustments: Quitting smoking, improving diet, and better oral hygiene.
- Medical monitoring: For patients with chronic illnesses, close coordination between dentists and doctors ensures infections are managed early.
Addressing the underlying issues can prevent minor problems from escalating into dangerous infections that threaten your teeth and overall health.
User Experience
1. One dentist on Quora, Dr. Murray Orr, explained that although deaths from tooth infections are rare, he has witnessed how dangerous they can become. He shared a case of a young man whose neck swelled so severely from an abscess that he couldn’t lower his chin. The condition, known as Ludwig’s Angina, was blocking his airway and required emergency hospital treatment, including surgery, drainage, and IV antibiotics, to save his life.
2. Another contributor, Ronald Leach, highlighted that an untreated tooth infection can turn deadly. Often, the tooth is painful at first, but once the nerve dies, the pain may disappear leading patients to think the problem is gone. In reality, swelling continues to spread, and if bacteria reach the bloodstream, it can trigger sepsis and organ failure, which can be fatal without urgent care.
3. Similarly, a Quora user named Melody VanHoose shared a tragic real-life example. She recalled a woman from her church who developed a simple toothache that rapidly worsened. Within just five days, the infection had spread toward her brain, and despite being otherwise healthy, she sadly lost her life.
Related FAQs
1. Can antibiotics cure a tooth infection permanently?
No. Antibiotics can control the spread of infection temporarily, but they don’t remove the infected tissue. A root canal or extraction is usually necessary for permanent resolution.
2. How do I know if my tooth infection has reached my bloodstream?
If you develop fever, chills, rapid heartbeat, or confusion, these may be signs of sepsis a medical emergency. Seek hospital care immediately.
3. Can a healthy person die from a tooth infection?
Yes. Even otherwise healthy individuals have died from untreated abscesses. While it’s less common, the risk is still real if treatment is delayed.
4. What’s the fastest treatment for an abscess?
The quickest relief comes from drainage either by incision or root canal therapy. Pain usually eases once the pus is released.
5. Can natural remedies ever replace dental care?
No. Natural remedies may help manage pain, but they cannot remove the source of infection. Only professional dental treatment can fully resolve a tooth abscess.
Conclusion
So, how long until a tooth infection kills you? The truth is, it varies sometimes infections remain localized for weeks, while in other cases, complications can arise in just a few days. What’s consistent is this: ignoring a tooth infection is never safe.
Modern dentistry makes treatment straightforward, whether through antibiotics, drainage, or root canal therapy. Prevention is even better daily oral hygiene, smart nutrition, and regular dental visits can keep infections at bay.
If you’re experiencing symptoms like swelling, fever, or difficulty breathing, don’t wait. Seek immediate dental or emergency care. Acting fast could save more than your tooth it could save your life.
Medical Disclaimer: This article is for informational purposes only and should not replace professional medical advice. Always consult with a healthcare provider before making changes to your diet or health routine.


